Bladder cancer
Summary/Epidemiology
Cancers of the urinary tree, or urothelial carcinomas, can develop in the bladder or ureters.
The bladder collects urine from both kidneys through the ureters; it is located in the lower part of the abdomen, just behind the pubis. Approximately 2500 new cases of bladder cancer are diagnosed in Belgium each year. This cancer is more common in men than in women and is usually diagnosed after the age of 60. Tobacco smoking is the main risk factor; prolonged exposure to toxic products (industries manufacturing paints, textiles, textile dyes, rubber, plastics, etc.) also increases the risk of bladder cancer. Other risk factors can sometimes be found, such as heredity, chronic bladder irritation, repeated infections, etc.
Urothelial carcinomas initially develop in the mucosa of the bladder (the most superficial layer of the bladder) or the ureters; the bladder is the most frequently affected site, while urothelial carcinoma of the ureter remains rare. Urothelial carcinomas of the bladder can grow superficially, not infiltrating the bladder muscle. These superficial tumors, if not treated promptly and completely, will spread deeply and infiltrate the bladder muscle. Cancer that invades the muscle can quickly spread outside the bladder and invade the lymph nodes around the bladder or send cancer cells to distant sites (metastasis).
Symptoms
Bladder cancer often manifests itself through the presence of visible blood in the urine. This symptom, which can also be observed in other diseases, requires a prompt medical consultation. A cystoscopy will then be performed and in case of a suspicious lesion, a biopsy will be carried out in order to retrieve a tissue sample for analysis.
Biopsy results confirm the diagnosis of urothelial carcinoma of the bladder and clarify whether it is a superficial cancer or a cancer infiltrating the bladder muscle.
Treatments
Superficial bladder cancers are treated by endoscopic resection (i.e. by cystoscopy, inside the bladder and leaving the bladder in place). Resection may be followed by injections, again inside the bladder, of chemotherapy products or inflammatory products such as Bacillus Calmette and Guerin (BCG), the purpose of which is, like immunotherapy, to trigger a major inflammatory reaction in order to stimulate the white blood cells to destroy the residual cancer cells. These bladder tumors require close monitoring by cystoscopy at regular intervals.
If the cancer invades the bladder muscle, treatment is more complex and requires several steps. The first step is to administer chemotherapy, an intravenous drug that kills fast-growing cells, to shrink the tumor and kill any cancer cells that may have escaped. After chemotherapy, a radical treatment of the bladder must be considered; it is either a complete surgical resection of the bladder (cystectomy) with derivation of the urine to the skin via a stoma or with construction of a 'neo-bladder'. An alternative to surgery may be bladder radiation therapy, which is the daily administration of radiation focused on the entire bladder for a specific period of time, in combination with chemotherapy. These different options are discussed in a multidisciplinary oncology consultation (MOC) where experts involved in the management of bladder cancer meet to define the best strategy. These different types of treatment (surgery/radiation therapy, stoma/neo-bladder) must be discussed thoroughly with your doctor and cannot be offered systematically to the patient.
In the presence of distant metastasis, that is to say in the case of advanced cancer, surgery is not considered in first intention and a treatment diffusing in the whole body is preferred. Two options are then possible, chemotherapy or immunotherapy; this choice will be decided according to the characteristics of the cancer in the biopsy.
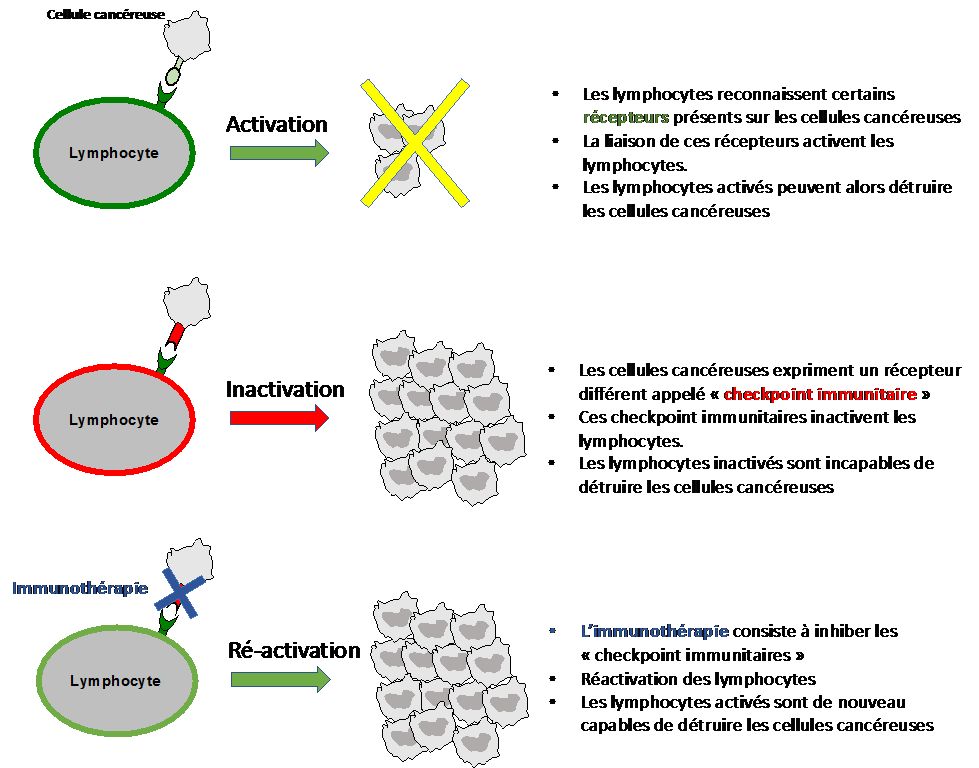
Immunotherapy has revolutionized oncology in general and is commonly used in kidney cancer. Our immune system is basically able to recognize and destroy cancer cells thanks to white blood cells and macrophages. However, cancer cells can adapt and develop defense mechanisms against our immune system, making themselves invisible to white blood cells (called immune escape). The goal of immunotherapy is thus to re-stimulate the immune system so that it is again able to recognize and destroy cancer cells. These molecules are administered intravenously every 2 to 3 weeks. Even if they are well tolerated, autoimmune adverse effects are to be expected (diarrhea, skin rash, thyroid or liver function disorders, etc.).
As therapeutic options are limited in bladder cancer, we are developing and participating in numerous research protocols to evaluate new molecules that are potentially effective in this type of cancer. Participating in such a clinical trial, where a promising molecule may be offered to you, increases the available treatment options
Contact
For any further information, or if you would like to make an appointment, please contact the Oncology Care Coordinator at + 32 2 764 35 44.
Doctor

Dr Laurence ANNET

Dr Hélène DANO

Dr Axel FEYAERTS

Pr Jean-Luc GALA

Dr Marco GIZZI

Dr Sofie HEYLEN

Pr François JAMAR

Pr Fréderic E. LECOUVET

Pr Renaud LHOMMEL

Pr Jean-Pascal MACHIELS

Pr Vassiliki PASOGLOU
Dr Barbara SCHMIDT
Pr Emmanuel SERONT

Dr Stéphane THIRY

Pr Bertrand TOMBAL

Dr Julien VAN DAMME

Dr Sandy VAN NIEUWENHOVE

Dr Ad VANDERMEULEN
Paramedical

Karoline AMANN

Naila EL IDRISSI

Kim HENQUIN

Monique KASA VUBU

Christine REMACLE

