Endometrial cancer

Summary/Epidemiology
The endometrium is the inner mucous membrane, or lining, of the body of the uterus. Endometrial cancer is more common than ovarian cancer.
Risk factors
The occurrence of endometrial cancer is favored by obesity, high blood pressure, and diabetes. It mostly affects older women, after the menopause.
There are familial forms of endometrial cancer, which are favored by mutations in DNA repair enzymes (other than BRCA) and are often associated with colorectal cancers (colon and rectum mainly). This familial predisposition to digestive and gynecological cancers (ovarian cancer is also more frequent in certain forms) is called Lynch syndrome. At the King Albert II Institute, a multidisciplinary group, including geneticists, oncologists, gastroenterologists, digestive surgeons, pathologists, and gynecologists, is specifically in charge of managing these women.
Symptoms
Endometrial cancer manifests as abnormal vaginal bleeding, even if minimal. The recurrence of vaginal bleeding in postmenopausal women or bleedings between periods in premenopausal women (rarer) is sometimes suggestive. These symptoms require a medical consultation in order to make a rapid diagnosis.
If the examinations are carried out as soon as the first symptoms appear, it is an early diagnosis, with a good prognosis in most cases.
Diagnosis
Endometrial cancer is diagnosed through biopsy.
Examinations
The examination consists of a biopsy. A small sample of the suspected area is taken and examined under a microscope. The sample is taken during an "endoscopy", or more precisely, a "hysteroscopy". During this procedure, a guide equipped with a small camera at its end is introduced through the vagina. It is performed without anesthesia during the consultation and is usually very well tolerated. At the Cliniques universitaires Saint-Luc, we use very thin endoscopes (i.e., cameras), 2mm in diameter, so that the examination is almost painless.
Treatments
Treatment for endometrial cancer usually consists of a hysterectomy or complete removal of the uterus. At the King Albert II Institute, this intervention has been performed for many years by laparoscopy. The removal of the uterus by laparoscopy, or coelioscopy, shortens the hospital stay to about four days. This technique requires a specific training and a great experience.
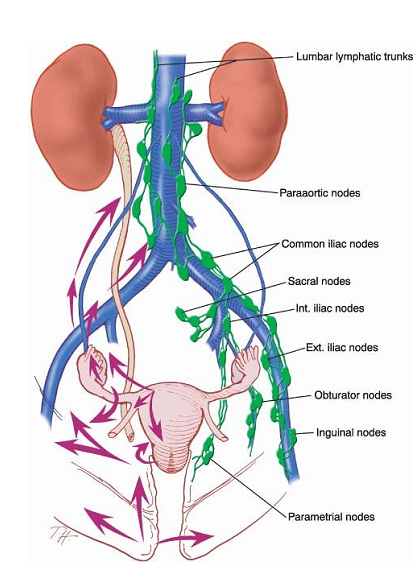
In some cases, if the tumor shows more aggressive characteristics or greater extension within the uterus, it is necessary to remove lymph nodes. Lymph nodes act as a filter for the lymph that circulates in the body. Lymph is the "excess" liquid that comes out of the vessels during blood exchanges in the organs to provide the cells with the nutrients and oxygen necessary for their survival. The lymphatic channels bring this excess liquid back to the bloodstream and contain, among others, the immune cells. The lymph nodes filter this liquid and retain abnormal cells, microbes, etc. to organize the body's defenses. Each organ is drained by its own lymphatic circuit and therefore by a particular lymphatic area. In pelvic cancers, these are the pelvic and lumbo-aortic lymph nodes, which follow the same trajectory as the blood vessels supplying the organ.
Opposite: Schematic anatomical representation of pelvic organ drainage – pelvic and lumbo-aortic chains
These lymph nodes are therefore removed in situations where they are considered to be at risk of being affected by cancerous cells, in order to determine the need for complementary treatments to surgery. At the Cliniques universitaires Saint-Luc, lymph nodes are also removed by laparoscopy, which offers a major advantage in reducing the surgical burden, without opening the abdomen. In addition, in order to reduce the number of nodes to be removed and to refine the analysis of the nodes, the sentinel node mapping technique is used in endometrial cancer. The underlying principle is that each lymph node chain has one or more nodes that first receive the lymph from the organ, and then distribute it to the other nodes. This technique is routinely used in breast cancer where it has been validated for several years, and the first studies carried out in endometrial cancer seem to show a benefit. The Cliniques universitaires Saint-Luc were at the forefront of the development of this technique and one of the first Walloon centers to apply it in endometrial cancers. It demands a particular experience and a learning curve. A multicenter observational study is currently being conducted in several centers in Belgium, initiated by the King Albert II Institute onco-pelvi group, of which they are the principal investigators.
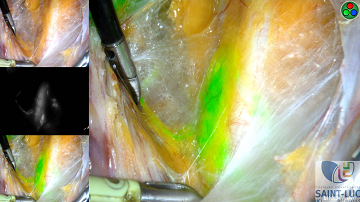 Opposite: Sentinel node visualized intraoperatively by a fluorescent dye (indocyanine green) injected into the uterus at the beginning of the surgery. The camera that allows seeing the fluorescent light is unique because it makes it possible to superimpose the fluorescent image on the laparoscopic image.
Opposite: Sentinel node visualized intraoperatively by a fluorescent dye (indocyanine green) injected into the uterus at the beginning of the surgery. The camera that allows seeing the fluorescent light is unique because it makes it possible to superimpose the fluorescent image on the laparoscopic image.
New techniques for improved detection of sentinel lymph nodes have emerged, with the use of a fluorescent marker. The Cliniques universitaires Saint-Luc were one of the first centers to use this technology in the detection of sentinel lymph nodes, with promising results.
Because endometrial cancers are diagnosed early in women who undergo regular gynecological examinations, they generally do not require additional treatment. Radiation therapy to the pelvis is sometimes undertaken when the tumor is at risk of recurrence. In case of lymph node involvement, chemotherapy followed by pelvic and sometimes lumbo-aortic radiation therapy are administered.
Guidelines, based on a consensus of the different European scientific organizations of physicians involved in the treatment of endometrial cancer (gynecologists, oncologists, and radiotherapists), were published in 2015. They were reviewed and discussed extensively by the physicians of the teams collaborating with the King Albert II Institute during a consensus meeting in 2017 and integrated into our own guidelines, ensuring that patients within the King Albert II Institute and its gynecological oncology network benefit from homogeneous management at the cutting edge of evidence-based medicine and scientific advances.
Conclusion
Optimal treatment requires a multidisciplinary and centralized approach. The frequent combination of the different therapeutic options of surgery, radiation therapy, and chemotherapy illustrates the need to correctly define the characteristics of the cancer. This approach makes it possible to establish the care plan and the sequence of treatments. This requires the cooperation of specialists in imaging or microscopy capable of assessing the aggressiveness of the cancer and its extent.
The weekly multidisciplinary meetings organized at the King Albert II Institute therefore include all the specialists involved in the diagnosis and treatment of gynecological tumors. They make it possible to identify the most appropriate therapeutic attitude for each patient, in accordance with current standards of care.
Contacts
Pour toute information complémentaire ou demande de rendez-vous, vous pouvez prendre contact avec une Coordinatrice de Soins en Oncologie au + 32 2 764 94 08.
Contacts
Doctor

Pr Jean-Francois BAURAIN

Dr Frank CORNELIS

Dr Sophie CVILIC
Dr Latifa FELLAH
Quitteries FONTANGES
Dr Aline FRANCOIS

Dr Amandine GERDAY

Dr Pascale JADOUL

Dr Carine KIRKOVE

Dr Isabelle LECONTE

Dr Mathieu LUYCKX
Dr Charlotte MAILLARD

Dr Filomena MAZZEO

Dr Vasiliki PERLEPE

Pr Jean-Luc SQUIFFLET
Paramedical

Laurence BEAUSAERT
Ingrid DE BIOURGE

Fanny DEPRÉ

Maëlle DETRY

Naila EL IDRISSI

Louise FAVARETTO

Florence FONTAINE

Monique KASA VUBU

