Prostate cancer

Summary/Epidemiology
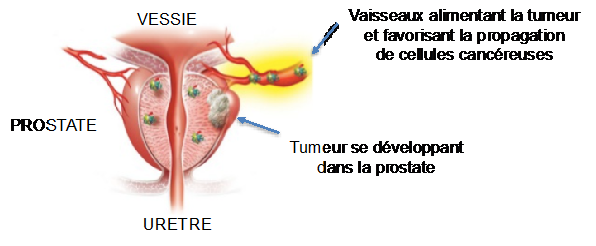
The prostate is a gland, the size and shape of a chestnut, located under the bladder and in front of the rectum. The role of the prostate is to produce a nutritive fluid in which the spermatozoa bathe. The development and function of the prostate is influenced by the testosterone produced by the testicles. With advancing age, the prostate increases in size and normal prostate cells may become cancerous due to an accumulation of errors during each cell division. Still stimulated by testosterone, these cancer cells gradually form a tumor that invades the prostate.
Prostate cancer is the most frequently diagnosed cancer in men. In Belgium, 9500 people are diagnosed with prostate cancer every year. The risk of prostate cancer increases with age, which is why it is mostly diagnosed after the age of 50. However, family history and environmental factors may promote its development at a younger age.
Compared to other cancers, prostate cancer generally has a better prognosis with a 5-year survival rate of over 90% for all stages. Indeed, many prostate cancers are slow-growing and may not cause symptoms or life-threatening clinical consequences. Moreover, since the majority of prostate cancers are diagnosed at the localized stage, current treatments are mostly curative.
It is of paramount importance that each patient with a diagnosis of prostate cancer be discussed in a multidisciplinary oncology consultation (MOC) bringing together the experts involved in its management: urology, oncology, radiation therapy, radiology, anatomopathology, and nuclear medicine. Our department complies with rigorous quality criteria in the management of prostate cancer and in this respect is part of the European network of excellence Prostate Cancer Unit. Prostate Cancer Unit.
Symptoms
Early prostate cancer does not cause any symptoms. It is therefore important not to wait for urinary symptoms to occur before seeking help. When urinary symptoms do occur, they are often the result of a benign, age-related swelling of the prostate gland (benign prostatic hyperplasia).
A more or less important invasion of the prostate gland can also lead to urinary manifestations. The presence of metastases, mainly bone metastases, can manifest itself in the form of a significant alteration of the general state of health with unexplained weight loss, but also bone pain (pain on mobilization or linked to movements), in the form of spontaneous fractures due to bone fragility, or in a completely asymptomatic way.
Screening
Screening aims to detect cancer before it causes symptoms, at an early, curable stage. Prostate cancer screening should be discussed between the patient, his general practitioner, and his urologist. Indeed, many prostate cancers are indolent cancers, evolving very slowly to an aggressive cancer and therefore requiring only a simple surveillance initially. However, as it is difficult to predict the evolution of the cancer, a radical treatment will be proposed and associated with significant adverse effects (incontinence, impotence, etc.) for a survival similar to that which would have resulted from a treatment started later.
Prostate cancer screening includes the measurement of the PSA (prostate-specific antigen) level in the blood. The PSA is a protein secreted by the glandular cells of the prostate, but also, and in greater quantities, by cancer cells; PSA is therefore unfortunately not specific to prostate cancer, which means that an increase in PSA can be due to another disease of the prostate, such as an infection or benign prostatic hyperplasia.
According to the guidelines of the Belgian Urological Association, it is recommended to discuss the usefulness of a first PSA test with men from the age of 50, after having discussed with them the advantages and disadvantages (see box “What messages should be given to men before they are screened?”). If there is a family history of prostate cancer or in African patients, PSA screening should be offered as early as age 45. On the other hand, there is no point in screening for prostate cancer in men with a life expectancy of less than 10 years (except, of course, in the case of symptoms).
What messages should be given to men before they are screened?
-
Screening for prostate cancer using digital rectal examination and PSA measurement reduces the risk of death from prostate cancer by 29%, but this risk remains low, at about 4 deaths per 1000 healthy men.
-
Screening can diagnose prostate cancer in its early stages, when the tumor is still localized to the prostate.
-
Early prostate cancer does not cause symptoms. Although urinary symptoms most often indicate benign prostatic hyperplasia, they can also be caused by advanced prostate cancer, which in most cases will not be curable. Therefore, it is important not to wait for the onset of symptoms to inform the patient.
-
If patients accept to undergo screening, they must
-
be aware of the risk of having one or more prostate biopsies to confirm the presence of cancer;
-
be aware of the risk of finding cancer cells that will not threaten their health. This is called indolent cancer.
-
These cancers are a source of great anxiety and can lead to aggressive treatments, which will result in complications, particularly incontinence and erectile dysfunction, that are not justified. One must accept the fact that prostate cancer treatments inevitably lead to adverse effects: incontinence and urinary disorders, alteration of sexual function, etc.; accept the fact that cancerous cells are found and that it is proposed to simply monitor it by performing repeated PSA measurements and, possibly, new biopsies.
-
Additional examinations
If the PSA is elevated, the doctor will perform a digital rectal exam and measure the volume of the prostate. By combining these three factors, he will be able to calculate the risk of prostate cancer, using simple computer tools available on the Internet.
If the risk of significant cancer exceeds 5%, the doctor will prescribe a prostate magnetic resonance imaging (MRI). This minimally invasive examination will allow to correctly visualize the prostate, measure its volume, and identify the presence of a suspicious lesion.
Prostate biopsy is the only test that can confirm the diagnosis of cancer and analyze its characteristics. Under ultrasound guidance, the urologist takes samples of suspected cancerous areas of the prostate gland by inserting a needle through the rectal wall. These cells are then examined under a microscope by an anatomopathologist to determine the characteristics of the cancer. The Gleason score, for example, is a score that measures how aggressive the cancer cells are; the higher the Gleason score, the more aggressive and rapidly proliferating the cancer is.
The Gleason score
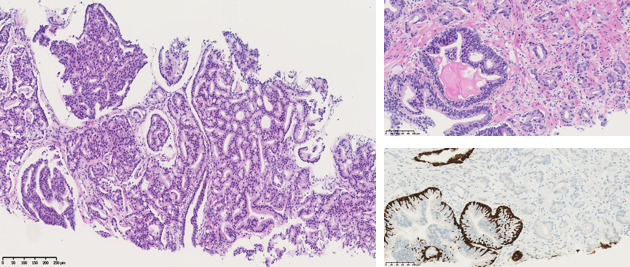
Classification of prostate cancers
Active surveillance is therefore a very good option for cancers with a Gleason score ≤ 6 and a PSA < 10 ng/ml. The recently published PIVOT trial demonstrated that immediate treatment with prostatectomy does not increase the chances of survival compared to surveillance alone.
Based on the PSA, digital rectal exam, and Gleason score, prostate cancers are classified as low, intermediate, high, or very high risk of progression. This classification will be used to decide with the patient what is the best treatment for the stage of his disease.
For high-risk cancers and in case of recurrence of the disease, the physician will prescribe additional examinations to ensure the absence of metastases and, where applicable, to monitor their evolution.
These examinations include:
- A bone scan that visualizes the entire skeleton, as prostate cancer mainly metastasizes to the bone.
- A total thoracoabdominal scan to exclude the presence of suspicious lesions in the lung or liver.
- A whole-body MRI, which allows in a single examination to visualize and study not only the prostate, but also the whole body.
- A PSMA PET-CT, performed in nuclear medicine, consists in injecting a special tracer that binds to PSMA, a particular protein specific to cancer cells, which allows identifying any cancerous lesion of prostatic origin in the entire body, even if it is millimetric.
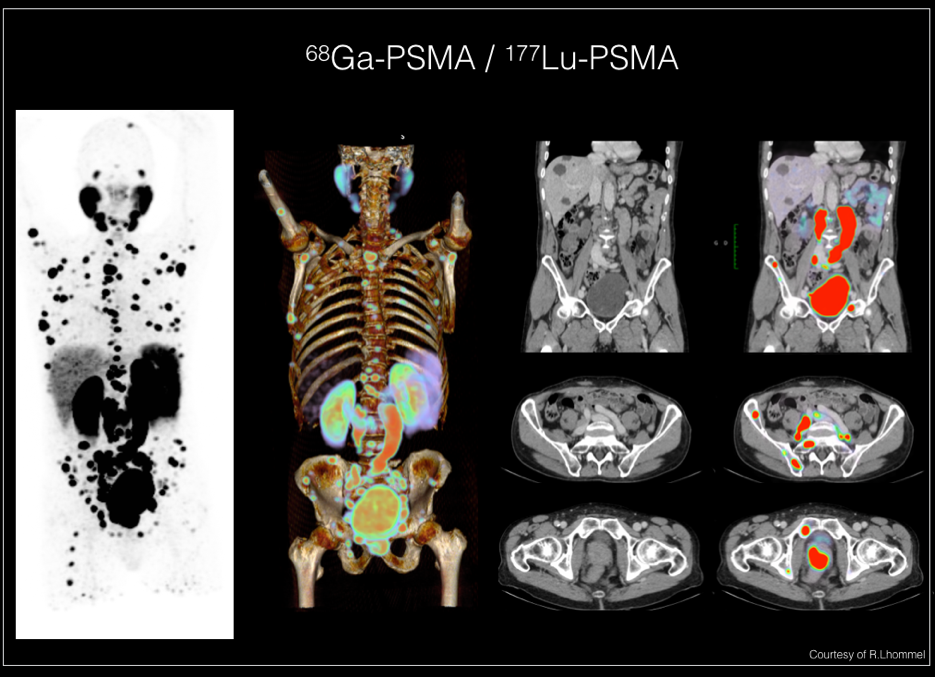
These imaging techniques are studied, compared, and continuously improved through medical research. In addition, we are developing numerous national and international protocols to confirm the place of these examinations in the standard management of prostate cancer.
Treatments
The treatment of prostate cancer depends on the risk of progression. Each cancer diagnosis and treatment suggestion is discussed in a multidisciplinary oncology consultation (MOC). When several strategies are possible, the doctor must discuss with the patient which strategy is best for him. Our department also offers the support of our oncology nurse coordinators and psychologists.
In the case of localized cancer, it is important to first decide whether treatment is absolutely necessary. Indeed, some prostate cancers remain indolent for years and progress very slowly. These are mainly prostate cancers with a low risk of progression (very small size, low Gleason score (<7), and a PSA of less than 10ng/ml); this type of cancer can then be monitored very regularly by PSA, MRI, and repeated prostate biopsies.
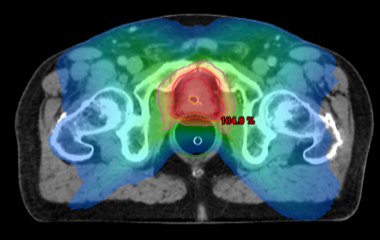
By contrast, intermediate and high risk cancers may progress more rapidly and radical treatment will be required, either by surgical removal (total radical prostatectomy) or by internal (brachytherapy) or external radiation therapy. In our center, the integration of multimodal imaging (CT or MRI) into the radiation therapy planning process, along with the intensity-modulated radiation technique (IMRT), allow the radiation to be guided to the tumor in an extremely precise manner, which increases the effectiveness of the treatment while avoiding damage to surrounding healthy tissue.
In case of very high risk cancer, i.e. with lymph node involvement, a combined treatment is proposed, combining radiotherapy and hormone therapy, or surgery followed by radiotherapy + hormone therapy.
All of these treatment options must be discussed between the patient and the various specialists involved in order to choose the most appropriate treatment (Counselling the patient with prostate cancer). Before choosing the treatment, it is essential to discuss the benefits, but also the various adverse effects that can alter the quality of life (incontinence, false needs, impotence, loss of libido) and their treatment.
In case of metastatic prostate cancer, which has already spread outside the prostate, most often to the bones, the reference treatment is to reduce the progression of male hormones that are involved in the growth of prostate cancer. Hormone therapy is given as a monthly, quarterly, or semi-annual injection. The adverse effects of hormone therapy can be bothersome and increase the risk of cardiovascular disease and osteoporosis (Counselling the patient with prostate cancer).
This hormone therapy stops the production of testosterone and allows the cancer to be controlled in 80 to 90% of patients. However, despite an initial response to hormone therapy, the cancer may adapt and progress again (this is called castration-resistant prostate cancer).
Fortunately, several new medications are available:
- New or "second generation" hormone therapies block the residual secretion of testosterone and prevent it from binding to the receptors present on the cancer cells. This category of drugs includes Zytiga®, Xtandi®, Erleada®, Nubeqa®, etc. These drugs are generally taken orally and continuously; they can be administered early or later in the disease course, depending on the extent of the cancer.
- Chemotherapies such as Taxotere® or Jevtana®. They are administered intravenously in the day hospital every 3 weeks. These molecules kill rapidly proliferating cells, mainly cancerous cells.
- A specific treatment for bone metastases, Radium-223 (Xofigo®), which is injected every month.
- Drugs that strengthen bones and limit complications related to bone metastases.
In recent years, new treatment strategies have been developed for metastatic prostate cancer. Several studies have shown that the combination of different treatments provides a clear survival benefit compared to a succession of these treatments. The first line of treatment for metastatic prostate cancer is therefore the combination of hormone therapy (castration) with chemotherapy or second generation hormone therapy.
Follow-up of patients on hormone therapy
Testosterone suppression therapy is the gold standard of systemic treatment for advanced prostate cancer. It lowers the testosterone levels, which results in a series of metabolic changes. Most adverse effects occur relatively quickly, within a few weeks of starting hormone therapy. Metabolic symptoms and osteoporosis may appear later.
Our department has developed an extensive program to assist patients receiving hormone therapy, the FEELplus program.
The following symptoms or syndromes are common in patients receiving hormone therapy:
- Fatigue, gloominess, malaise, depression
- Decreased libido, loss of interest in sex
- Reduction of hair growth
- Hot flashes: this is the adverse effect often reported as the most annoying by patients. Among the medical treatments that have demonstrated some effectiveness, there are: clonidine (Dixarit®), medroxyprogesterone acetate (Provera®), cyproterone acetate (Androcur® or Cyproplex®), and certain antidepressants such as venlafaxine or fluoxetine (Prozac® and generics). In addition, sage and evening primrose oil can also provide relief.
- Gynecomastia (painful swelling of the breasts). In this case, two sessions of radiation therapy of the mammary gland give good results.
- Muscle wasting and muscle weakness. The best way to limit the impact of this sarcopenia is the regular practice of light resistance training, adapted to the patient's physical condition.
- Anemia
- Metabolic disorders. Hormone therapy by medical or surgical castration is associated with an increased risk of diabetes, metabolic syndrome, and cardiovascular disease. It is important to adapt existing treatments or even start a new treatment depending on the patient's evolution. Cardiovascular disease is the leading cause of death in patients on hormone therapy. In patients who do not have metastatic disease at the time of treatment initiation, the risk of death from cardiovascular disease is greater than the risk of death from prostate cancer.
- Osteoporosis and pathological fractures. As in menopausal women, the decrease in hormones can lead to bone loss, which can result in osteoporosis. This increases the risk of fracture. It is important to ensure that the patient is properly supplemented with calcium and vitamin D. If risk factors are present, it is useful to ask for a bone densitometry at the beginning of the treatment.
Research and quality of care
Research is obviously essential in order to identify potential biomarkers predictive of the efficacy or inefficacy of a particular molecule. As a center of expertise, we encourage and stimulate participation in clinical research protocols, in very close collaboration with other national and international centers, in order to provide today's patients with the opportunity to receive tomorrow's treatment. Although standard treatments are available, we will not hesitate to offer the opportunity to participate in the clinical evaluation of a new drug that could revolutionize oncology.
Our role is to help the patient through the various steps from screening to treatment. Each specialist (urologist, radiologist, oncologist, radiotherapist, anatomopathologist) has a specific role in this care. Fortunately, our nurse coordinators provide personalized support for patients from one specialty to the next, being available to answer the smallest of questions and ensuring quality follow-up throughout the treatment, a presence in case of questions and help in case of problems. For example, hormone therapy or castration can sometimes be physically and emotionally difficult. Indeed, the deprivation of male hormones leads not only to impotence and loss of libido, but also to longer term adverse effects such as weight gain, osteoporosis, and cardiovascular problems. A whole team is there to help the patient. Thanks to the medical research of our center, we try to establish new strategies in order to limit these adverse effects (communication, physiotherapy support programs, dietary assistance, etc.). Psychological help is also systematically offered to support any patient in the difficulties encountered during this journey. In elderly patients, a geriatric evaluation is systematically performed. If this assessment reveals frailties, geriatric interventions and modulation of the cancer treatment are proposed with the collaboration of our geriatric colleagues, in order to ensure an adapted and personalized care of the patient.
Contact
For any further information, or if you would like to make an appointment, please contact the Oncology Care Coordinator at + 32 2 764 35 44.
Doctor

Dr Laurence ANNET

Dr Hélène DANO

Dr Axel FEYAERTS

Pr Jean-Luc GALA

Dr Marco GIZZI

Dr Sofie HEYLEN

Pr François JAMAR

Pr Fréderic E. LECOUVET

Pr Renaud LHOMMEL

Pr Jean-Pascal MACHIELS

Pr Vassiliki PASOGLOU
Dr Barbara SCHMIDT
Pr Emmanuel SERONT

Dr Stéphane THIRY

Pr Bertrand TOMBAL

Dr Julien VAN DAMME

Dr Sandy VAN NIEUWENHOVE

Dr Ad VANDERMEULEN
Paramedical

Karoline AMANN

Naila EL IDRISSI

Kim HENQUIN

Monique KASA VUBU

Christine REMACLE

